Cardiovascular
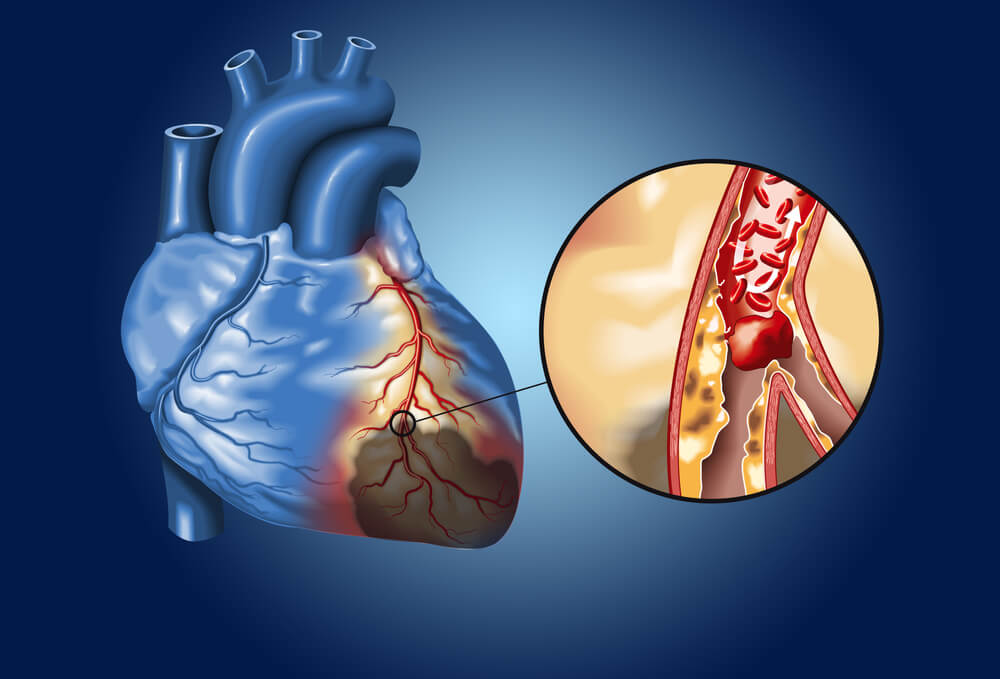
Atherosclerotic Coronary Artery Disease Management:
Atherosclerotic coronary artery disease (ASCAD) demands vigilant medical care. Following a heart attack, comprehensive post-MI (myocardial infarction) strategies involve lifestyle modifications, medication management & adherence, and cardiac rehabilitation. Similarly, after intra-arterial stent placement or coronary artery bypass grafting (CABG) surgery, ongoing management focuses on preventing further plaque build-up, regular cardiac monitoring, and medication compliance. These interventions aim to ensure optimal heart health and reduce the risk of recurrent cardiovascular events.

Angina Pectoris:
Angina pectoris, characterized by substernal chest pain, necessitates a multifaceted approach to diagnose & alleviate symptoms and prevent complications. Medications, lifestyle adjustments, and stress management play pivotal roles in angina pectoris management. Regular medical evaluations and a collaborative patient-doctor relationship are crucial for tailoring an effective care plan that addresses the underlying causes and triggers of chest pain.
Hypertension:
Effectively managing hypertension (high blood pressure) involves lifestyle modifications such as a heart-healthy diet with low sodium, regular exercise, and stress reduction, complemented by antihypertensive medications. There are little to no symptoms of hypertension. Therefore, routine blood pressure monitoring at home and at regular medical check-ups are essential for adjusting treatment plans to maintain optimal blood pressure readings and prevent long-term complications.


Hyperlipidemia:
Managing hyperlipidemia, characterized by high cholesterol levels, necessitates dietary changes, regular exercise, and medication adherence. Maintaining low LDL & triglyceride levels, and high HDL levels should be the goal. Lifestyle modifications & a low fat diet aim to lower cholesterol and reduce the risk of atherosclerosis and related cardiovascular issues. Regular fasting lipid profile laboratory assessments and medication adjustments contribute to long-term heart health.
Atrial Fibrillation:
Managing the irregular heart rhythm of atrial fibrillation involves a combination of rhythm management, heart rate control, and consideration for anticoagulation. In some cases, the placement of a permanent pacemaker or Watchman device is used. Regular monitoring of heart rate & rhythm, lifestyle modifications, and medication compliance are crucial for preventing complications such as stroke or embolism and improving overall quality of life.


Valvular Heart Disease:
Valvular heart disease (VHD), including post-valve replacement of the aortic or mitral heart valves from either transcatheter or open heart surgery, requires meticulous follow-up care. This includes regular echocardiograms, anticoagulation therapy if needed, and close examinations for potential complications. Regular monitoring and medication adherence contribute to maintaining optimal heart function and preventing further heart valve-related issues.
Peripheral Vascular Disease:
Peripheral vascular disease (PVD), marked by blockages in veins and arteries of the legs or arms causing pain from the ischemia, demands a quick & comprehensive medical approach. Lifestyle modifications such as stopping smoking, medications, and, in some cases, intravascular procedures aim to alleviate symptoms of ischemia and improve blood flow. Regular vascular assessments and ongoing management are vital to prevent complications and enhance overall circulatory health.

